What is IBS?
IBS is a disorder of gut-brain interaction (DGBI), meaning the bowel and digestive system are physically healthy, with no damage, inflammation, or structural changes. Instead, the communication between the gut and brain is disrupted, leading to altered sensations and digestive functions.
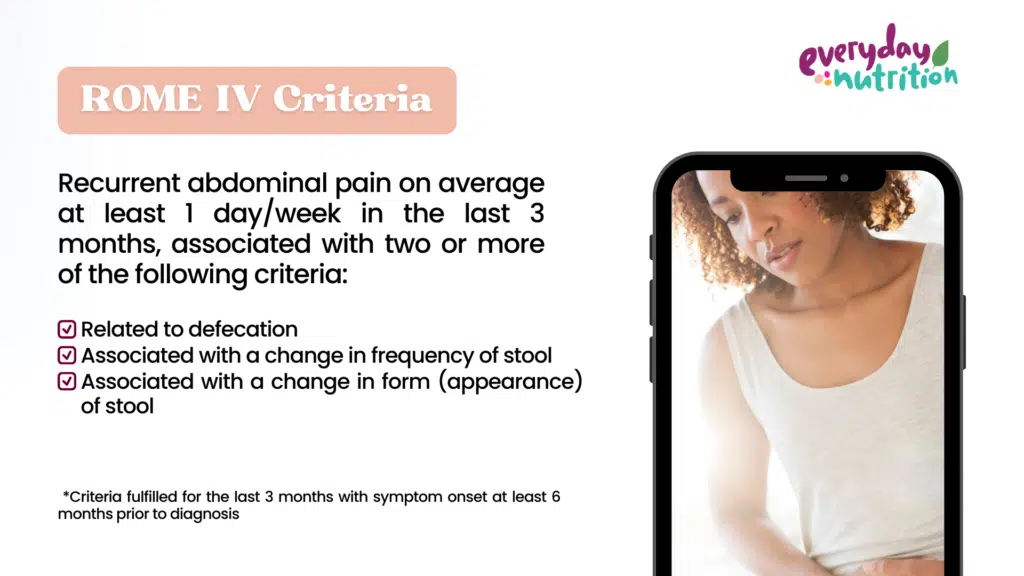
There is no blood test or diagnostic procedure that can identify IBS, instead these are used to exclude other reasons for your symptoms, and then diagnosis is made based on the ROME IV criteria.
There are many conditions which cause similar symptoms to IBS, including Coeliac Disease, Inflammatory Bowel Disease (Crohn’s and Colitis) and even some cancers. It is essential to rule these out and investigate any “red flags” before exploring dietary modifications.
Once your doctor has determined that you do not have a medical condition that requires treatment, the next step is to be assessed by a dietitian. An experienced dietitian will assess your diet, your symptoms and your lifestyle to determine the best therapeutic diet to treat your symptoms. He or she will guide you through pinpointing specific trigger foods, implementing any dietary changes, and will ensure your diet remains balanced through out the process.
Over the last 25+ years I have worked in healthcare, I have learnt that the first step of creating an effective and safe plan, is knowing what you are treating.
Science doesn’t know exactly what causes IBS, but we know that the sensitivity of the nerve endings and the gut brain axis play an important role. You can read more about the gut brain axis here
We also know that certain lifestyle and dietary factors that can trigger attacks in susceptible people, and a management plan that considers a combination of approaches generally gives best symptom relief.
Medical Nutrition Therapy
Its now well documented that Medical Nutrition Therapy (MNT) can minimise IBS symptoms and prevent flare ups. MNT is implemented by an Accredited Practising Dietitian (in Australia) or a Registered Dietitian (In other parts of the world). The dietitian will assess your symptoms, your diet, your suspected triggers (if there are any) and your medical needs, to determine what type of intervention is right for you. Therapeutic diets may include:
- A low FODMAP diet
- The Royal Prince Alfred Hospital (RPAH) elimination diet to assess sensitivity to naturally occurring food chemicals (salicylates, amines and glutamates)
- Whole food elimination diet to assess sensitivity to wheat, dairy, soy, eggs or
Most of the this will involve a structured elimination process for 2-6 weeks followed by systematic food reintroductions to identify problematic foods or food groups.
There are many tests that are advertised as being able to identify food intolerances, however most of them are expensive, misleading and unreliable. You can read more about these tests from the Australian Society for Clinical Immunology and Allergy
General diet
A low fibre diet can exacerbate IBS. Fibre isn’t digested by the body and passes through the gastro-intestinal tract relatively intact. It adds bulk to stool, increasing the size and weight as well as softening it. A bulky stool will always be easier to pass and reduce the risk of constipation. If you have diarrhoea, certain types of fibre will also absorb some of the liquid and solidify the stool, making it less watery. With IBS, tolerance and symptom management is often all about the types of fibre.
Stress
Visceral hypersensitivity and the gut brain axis play a large role in IBS. Put simply, visceral hypersensitivity is when the nerve endings in and around the gut are on high alert and respond very quickly to movement or stretching in and around in the gut. The low FODMAP diet aims to prevent this by minimising the types of foods that are fermented in the colon (causing gas and bubbles in the process). Other strategies include using mindfulness, meditation, light exercise and other relaxation techniques that are beneficial for winding down the entire nervous system, help increase your tolerance for trigger foods, and make managing IBS more achievable.
Eating behaviours
Size of meals and speed of eating also have an impact on IBS symptoms. Eating too quickly results in eating too much and the swallowing of excess air, which will exacerbate gut symptoms. Aiming for small regular meals and chewing thoroughly (digestion begins in the mouth) can prevent over eating and reduce the amount of air and gas in the gastro-intestinal tract at any one time. Mindful eating is also a great way to really start enjoying your food and make it pleasurable again, within the confines of dietary restriction.
Gut irritants
Coffee, tea, alcohol, spicy foods carbonated drinks and chewing gum are all gut irritants. They may or may not be related to a food intolerance but in high doses can mimic or exacerbates IBS symptoms. Its best to consume these foods in moderation, and keep intake stable day to day e.g. 1 coffee per day rather than 5 on one day and none on the next. If you do have persistent symptoms despite being vigilant in other areas, you may want to minimise these types of foods and drinks.
Exercise
The benefits of regular exercise are far reaching and beneficial on so many levels. In terms of IBS, light exercise can aid digestion and metabolism, it is a natural stress reliever and mood lifter. It doesn’t really matter what you do, it’s the movement, sustainability and enjoyment that are the important factors. Exercise ideas include walking, running, swimming, dancing, yoga, stretching, climbing on stuff or even just playing with your children.
Final Thoughts
Although IBS can’t be cured, it can be well managed and its effect on daily life minimised. A dietitian with expertise in functional gastro-intestinal conditions can help you put together an effective management plan so you can enjoy life without IBS getting in the way.
At Everyday Nutrition all our dietitians are gut health experts. We have the knowledge and experience help you resolve digestive issues and make peace with food. Book an appointment here to take back control of your gut and start enjoying life again.








3 Comments