The low FODMAP diet has been scientifically proven to help up to 80% of people find relief from symptoms of gas, bloating, abdominal pain and altered bowels. At this time, it is the most well researched and most effective approach for Irritable Bowel Syndrome (IBS). But what is a low FODMAP diet and how do you follow it?
This article will cover:
- What are FODMAPs and how they cause symptoms
- What type of symptoms are FODMAPs implicated in
- Examples of foods that contain FODMAPs
- How to identify your own food triggers using a low FODMAP diet
- The time frame form eating a food with FODMAPs to when it causes symptoms
- More detail on each FODMAP group
What are FODMAPs?
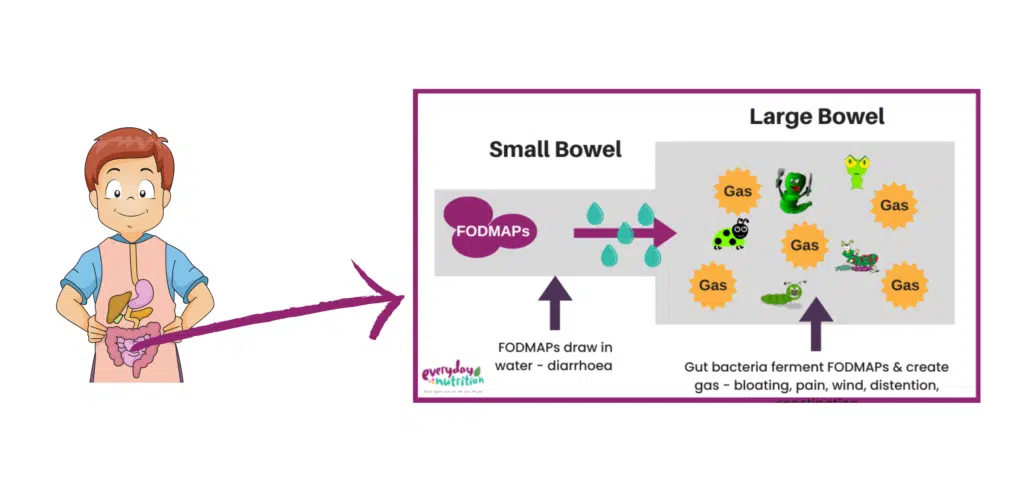
FODMAP is an acronym for four groups of short chain carbohydrates, or sugar molecules found naturally a variety of fruits, vegetables, grains, legumes and milk products. When we consume FODMAPs in food or drinks they are not digested properly in the small intestine. Instead, they stay in the digestive tract and continue their path to the large intestine (colon). It’s here in the large intestine that two processes occur that may trigger symptoms in certain people:
- Certain FODMAPs are highly osmotic (they draw water into the intestine). Because of this, they create pressure within the gut, and often cause diarrhoea.
- FODMAPs are fermented by the bacteria that naturally live in the large intestine, which can create large volumes of gas. For those with sensitive nerve endings (i.e. IBS) this can result in abdominal distention, bloating and cramping.
Although FODMAPs may contribute to IBS type symptoms, they are not dangerous and do not cause harm to the body or shorten lifespan. In fact, mild fluctuations in symptoms from day to day are reflective of a healthy and balanced diet that is nourishing your gut microbiome. If symptoms are excessive they can however be painful and impact on quality of life. If this is you, a low FODMAP diet may be worth trailing to see if it reduces the severity of your symptoms.
Symptoms:
Common symptoms that a low FODMAP diet may help with include:
- Bloating
- Pain
- Excessive gas
- Alternating bowels e.g. constipation or diarrhoea
It’s important to note that these symptoms can overlap with other more serious conditions e.g. coeliac disease, inflammatory bowel disease (Crohn’s or Colitis), endometriosis or bowel cancer. It’s important to discuss your symptoms with your doctor and exclude these before you change your diet
What foods contain FODMAPs?
| Fermentable | Carbohydrate (or sugar) molecules that can be fermented in the large intestine, creating IBS symptoms |
Oligosaccharides | Chain-length molecules including Fructans & GOS found in onion, garlic, wheat, barley, rye, inulin, legumes and some dried fruit |
Disaccharides | Lactose is a disaccharide found in milk, yoghurt, some soft cheese’s (ricotta), ice cream, custard and cream. Note: regular cheese and butter are naturally lactose free |
Monosaccharides | Fructose is a monosaccharide found in excess in some fruits, vegetables, juices, dried fruits and sweeteners (e.g. Honey, agave or high fructose corn syrup) |
And Polyols | Sugar alcohols (not like alcohol you drink) including Sorbitol & Mannitol found in cauliflower, mushrooms, stone fruit, apples, pears and certain artificially sweetened products e.g. protein bars, sugar free mints and gums. |
Identifying food triggers
Food triggers can be tricky to diagnose. Other than food elimination and challenges, there are no evidence based tests that reliably identify if you are sensitive to FODMAPs or what your threshold is for them.
Most people are not sensitive to all of the FODMAP groups, and since limiting FODMAPs restricts nourishment to your healthy gut bacteria it is not recommended to follow a low FODMAP diet indefinitely. For this reason, the low FODMAP diet is conducted in three phases.
Phase One | Phase Two | Phase Three |
Low FODMAP Phase: This phase lasts 2-6 weeks. During this time, you will avoid foods high in all FODMAP groups, so that you can assess your overall response to the low FODMAP diet
| Reintroduction phase: Your dietitian guides FODMAP challenges to determine your threshold for each FODMAP. This phase needs to be well structured and challenge foods need to be chosen carefully to get clear results. | Personalised diet: Once you know your thresholds, your dietitian can help you reintroduce some higher FODMAP foods. This stage ensures maximum variety, minimum symptoms and of course a healthy gut! |
How long do FODMAPs take to trigger gut symptoms?
FODMAPs must travel from the mouth through almost the whole of the digestive tract to the large intestine (the very last part before they leave the body) where they are fermented by the bacteria that live there. This takes on average 4-24 hours before symptoms can be expected. Many people get surprises about what foods they are sensitive to during the FODMAP process. So in the initial phases it’s good to keep an open mind and wait until the Challenge phase to identify trigger foods.
Oligosaccharides
Oligosaccharides are the ‘O’ of FODMAP. “Oligo” means “few” and “saccharide” means sugar. These molecules made up of chain lengths of individual sugars bound tightly together.
They include:
Fructo-oligiosaccharides (Fructans or FOS): Found in many fruits, vegetables, dried fruit and grains (wheat, rye, barley).

- Galacto-oligiosaccharides (Galactans or GOS): Found in legumes (kidney beans, lentils, chickpeas, soy beans) and some nuts.

Humans are not able to break down chains of Oligosaccharides, meaning that they are a FODMAP for everyone. Sensitivity to these is more about the sensitivity of the gut and the gut brain axis. Each person’s tolerance to Fructans and GOS will vary, depending on a number of issues:
- The individual person, their gut flora and how their gut is behaving on that day
- The amount eaten (in a sitting / over the day / over a number of days)
Disaccharides
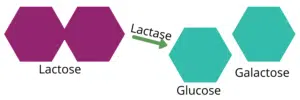
The Disaccharide or the “D” of the FODMAP acronym is lactose. Lactose is a double sugar molecule found in milk and milk products. However, not all dairy products are contain lactose and you will only need to avoid high Lactose products during phase 1 of the low FODMAP diet.
Low FODMAP dairy products include lactose free milk, yoghurt, ice cream and cream. Cheese and butter are already lactose free and you do not need to purchase specialty products. However, with lactose free products, make sure to check for high FODMAP additives e.g. fruit flavours, sweeteners or inulin.
Lactase enzymes can be purchased from the chemist or pharmacy. These can be either added as drops to milk or taken orally in tablet/capsule form with a food that contains lactose. The enzyme breaks down the lactose making the product easy to digest. These are very effective and handy to carry when out and about.
Nb: check the ingredients list as some lactase enzymes contain high FODMAP sweeteners or polyols
Monosaccharides (Excess fructose)
The monosaccharide or “M” of the FODMAP acronym is fructose. Fructose is a single sugar molecule that is present mostly in a range of fruits and vegetables. The key thing about Fructose is that glucose helps to absorb it, and it is only high FODMAP when in excess of glucose:
- Fructose < or = glucose (e.g. table sugar, orange, kiwi) = low FODMAP
- Fructose > glucose (e.g. apple, pear, mango, honey) = high FODMAP
We used to think that adding a glucose tablet to a high fructose food may help prevent symptoms, however, research has indicated that although it sounds possible, in practise, it doesn’t appear to work.
It is easy for fruit to add up when you at large serve. Although, you can eat several serves of fruit each day, space this out, and keep your intake of fruit to one standard “serve” per sitting
And Polyols
Polyols are sugar alcohols, not like the alcohol that you drink, but due to their chemical structure. Sorbitol and Mannitol are the are two main types of polyols found naturally in foods. You may also see ingredients like xylitol, maltitol, lactitol or isomalt listed on ingredients lists. These are also polyols and are considered high fodmap.
Most people do not absorb polyols properly. Polyols have a sweet flavour, but since they are not absorbed they don’t contain calories. This makes them great for artificially sweetening low calorie gums and mints. Polyols are also found naturally in certain fruits & vegetables.
Final Thoughts
Research shows that people who are guided by a FODMAP trained dietitian get better results, faster and restrict less food to achieve results. Not only that, but they save money at the supermarket, because they are more confident in choosing foods that are suitable. At Everyday Nutrition all our dietitians are Monash trained in the low FODMAP diet. Book an appointment here to take back control of your gut and start enjoying life again.








2 Comments